From TMH-NICE to ResTOR: An Eventful Journey A Treatise of developing a Tumor Megaprosthesis
Vol 1 | Issue 1 | May – August 2015 | page:40-44 | Ravi Sarangapani[1*].
Author: Ravi Sarangapani[1*].
[1]Development & Quality Director Adler Mediequip Pvt. Ltd, Pune, India.
Address of Correspondence
Mr. Ravi Sarangapani
Development & Quality Director, Adler Mediequip Pvt. Ltd., Sushrut House, Survey 288,
Next to MIDC Hinjewadi Phase II, At. Mann, Tal. Mulshi, Pune 411057, Maharashtra, India.
Email: ravi-sarangapani@adlermediequip.com
Abstract
The primary option for patients with osteosarcoma for many decades was an amputation to save life. A review in 1986 demonstrated that limb salvage surgery was as safe as an amputation and provided the evidence to change the surgical management of these patients to limb salvage surgery and megaprosthetic reconstruction. International developments since the 1990s formed the backdrop for the evolution of limb salvage surgery in India. Initial obstacles faced in India were that of patient affordability. In the late nineties, Dr. Ajay Puri and Dr. Manish Agarwal from the orthopaedic oncology department of Tata Memorial Hospital (Mumbai) in association with Sushrut-Adler initiated development of an indigenous limb salvage megaprosthesis (the TMH-NICE). This had to be a low-cost prosthesis by all means. This surgeon industry partnership over time led to overcoming many challenges and failures and continuous learning both on the clinical and engineering fronts resulting in the evolution of the ResTOR modular resection prosthesis system. This journey continues with improvements and modernization of the system contributing to cost-effective limb salvage surgery to patients in India and a number of other countries.
Keywords: Bone Tumor, Osteosarcoma, Limb Salvage, TMH-NICE, ResTOR.
Introduction
Although bone tumours form less than 1% of cancers in adults, they account for 3-5% of cancers in children with osteosarcoma being the most commonly diagnosed form of primary malignant bone tumours, followed by Ewing’s sarcoma [1]. These tumours represent the fourth most common type of cancer in patients under the age of 25.
The primary recourse for these patients for many decades was an amputation with an emphasis on sacrifice of the limb to save life. It was a landmark retrospective review by Simon et al in 1986 that demonstrated that limb salvage surgery was as safe as an amputation and provided the evidence that enabled surgeons to change the surgical management of these patients to limb salvage surgery and megaprosthetic reconstruction [2]. Enneking’s work related to staging of the disease [3] and the importance of surgical margins [4] significantly contributed to the development of limb-salvage surgery.
Not unlike most modern developments in the medical field, the clinical research and evolution of this treatment modality originated in the western world and resulted in limb salvage surgery with a megaprosthetic reconstruction slowly acquiring the status of “standard of care” for the majority of bone tumour patients through the 1990s. These International developments form the backdrop for what can aptly be termed the evolution of limb salvage surgery in India.
Indian Perspective
In late 1999, the Tata Memorial Hospital which is a pioneering initiative in the field of cancer care and research, originally commissioned in 1941, decided to augment their orthopaedic oncology service by bringing in a specialist orthopaedic surgeon to work with Dr. Badhwar, the then surgical oncologist who was also handling bone tumours. This resulted in Dr. Ajay Puri joining the oncology service of Tata Memorial in November 1999. Fate perhaps conspired in creating what would turn out to be a great team as Dr. Badhwar unfortunately took ill and the Tata Memorial management decided to recruit a second orthopaedic surgeon in the form of Dr. Manish Agarwal who came on board in January 2000. (read all about these happenings in the guest editorial by Dr A. Puri in this very issue [5]). Thus, two young and enthusiastic orthopaedic surgeons, well recognized in Mumbai for the contribution to the trauma service at major public hospitals, came on board to develop the orthopaedic oncology service at the Tata Memorial Hospital.
What Dr. Puri and Dr. Agarwal lacked in formal oncology training, they more than made up with their eagerness to learn, their obvious intelligence and most of all their dedication and commitment to make a difference to the lives of patients’ afflicted with this dreaded disease. The challenges they faced were numerous and perhaps too many to enlist; a gigantic workload of patients, a general lack of awareness of bone tumours and their management in the community, patient expectations, sometimes unrealistic to save limbs considering the social stigma attached to amputation considering the general difficulties faced by amputees in a developing country like India [6] and above all fast-advancing international developments in the management of bone tumours and perhaps frustration at not being able to offer the best standard of care to their patients. What they had in their favour was the backing and belief of the Institution, excellent infrastructure and the potential to form a world-class multi-disciplinary team.
As the development of the orthopaedic oncology service in Tata Memorial Hospital in the last fifteen years amply demonstrates, the selection panel which included Prof. Laud and Prof. Bawdekar and Dr. Dinshaw, the then Director of the Institution who also created these positions, did well. The young team, not fazed by the enormity of the challenges confronting them, set about tackling the problems they saw in a methodical and systematic manner.
One of their first priorities was to bring themselves up to date with the current international standard of care which involved offering their patients the option of limb salvage surgery with megaprosthetic reconstruction. As they started efforts to implement this initiative, they were faced with an obstacle not uncommon to the developing world, that of patient affordability. As so eloquently described by Dr. Agarwal and Dr. Puri, “Though all these exciting developments occurred in the West, in our own country limb salvage was still a difficult proposition. Chemotherapeutic drugs were very expensive, endoprosthesis unaffordable, ignorance widespread and the patients poor” [7]. This situation resulted in the team not being able to effectively offer the option of a good quality mega-prosthetic replacement to even ten patients of the approximately 200 new cases [7] or primary malignant bone tumours presenting to the hospital at that time.
It is said that experience can sometimes be a hindrance and the enthusiasm of youth goes a long way in surmounting seemingly impossible hurdles. The young team refused to be dismayed with these setbacks and set about convincing the management of the Sushrut-Adler Group (currently Adler Mediequip Pvt. Ltd., a Smith & Nephew subsidiary) of their mission to save limbs and improve the quality of life of these patients. It is testimony to their eloquence and persuasive skills that the Sushrut-Adler management adopted the surgeons’ goals as their own and agreed to invest the time and resources needed in the service of these patients, in a situation where a financially viable business was nowhere in sight. Thus began the evolutionary journey which took this Indian designed, Made-in-India implant from the early hesitant efforts of the TMH-NICE to the modular resection system, the ResTOR.
The Sushrut-Adler team commenced work, fabricating implants to patient dimensions in a surgeon-led design effort that was blessed by the Institutional Review Board of the Tata Memorial Hospital. In keeping with the objectives defined by Dr. Puri and Dr. Agarwal, the primary consideration was their estimate of what patient’s would be able to afford based on their understanding of the financial situation of these patients. This resulted in certain choices of material and fabrication methods which in hindsight were incorrect choices driven by the early “cost” objectives.
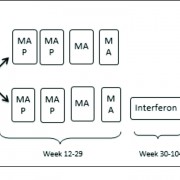
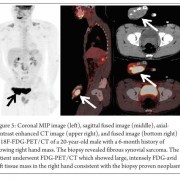
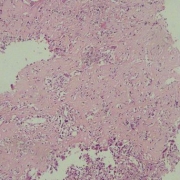
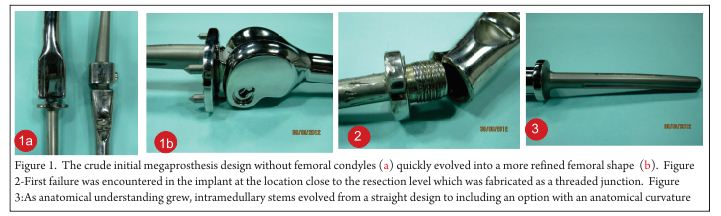
The early period between the years 2000 to 2002 featured implants that were almost entirely fabricated in a custom-basis to patient specific dimensions specified by the surgeon team. The rather crude initial design without femoral condyles (Fig.1a) quickly evolved into a more refined femoral shape (Fig. 1b) under the guidance of the surgeons. These implants were manufactured from 316L stainless steel, the material choice dictated by easy availability, ease of fabrication and cost considerations. The condylar region with the patient specific resection length was welded to the straight intramedullary stem which featured a male thread screwed into the resection shaft. Longitudinal grooves were machined into the stem to inter-digitate with bone cement and a valgus angle of 7 degrees was incorporated. The hinge pin was locked into place using a simple slotted screw.
In a first hint of problems to be faced in the future near the level of the resection or the intramedullary stem junction, a case of failure was encountered in the implant at the location close to the resection level which was fabricated as a threaded junction (Fig.2). This failure was similar to the failure of a humeral implant reported by Bos et al with a fracture at the base of a threaded stem [8] due to stress concentration and a structural weakness.
As the number of operated patients increased, the surgeons began to note certain repetitive dimensions that could be standardized. These were the Antero-posterior and Medio-lateral dimensions of the femoral and tibial condyles. Later on as the project progressed, other dimensions including stem diameters, lengths and types, lengths of resection segments and spacers would get standardized to enable modularity. The standardized condylar dimensions in 2002 enabled the femoral condylar section of the implant to be “cast” in 316L stainless steel, a development that featured in the implants manufactured in the period 2002-2004. The adoption of casting enabled some reduction in lead time by reducing the rather extensive condylar machining that was required earlier. As anatomical understanding grew, intramedullary stems evolved from a straight design to including an option with an anatomical curvature (Fig. 3).
It was also in this period that the first instrument set (Fig. 4) was created. Notably, nearly all surgeries performed by the surgeon team till that time had been carried out by using general orthopaedic instrumentation. With increasing experience came the realization that specifically designed instrumentation would be needed. Also contributing to this development was the fledgling thought in the minds of the surgeons that this system might go out of Tata Memorial Hospital some day in the future and it was important to create instrumentation that would enable easier use of this system by average surgeons. In late 2004, a circumferential groove oriented transversely (Fig. 5a) was added to the stem with the thought of improving cement fixation. This change resulted in early failure at the location of the groove (Fig.5b) and was quickly abandoned.
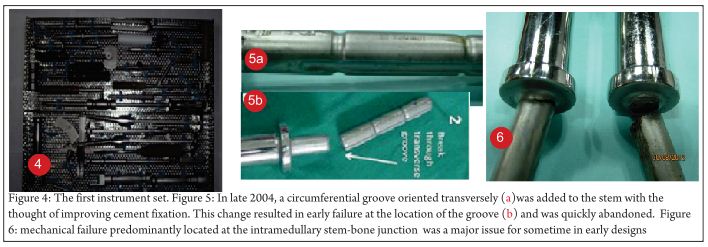
It was in early 2004 that the project began to face what would turn out to be its most major challenge, the incidence of mechanical failure predominantly located at the intramedullary stem-bone junction (Fig. 6). As subsequently reported in 2010 by Dr. Agarwal and Dr. Puri, there were 22 mechanical failures in 183 patients (12.02%) predominantly at the stem-collar junction with an average time to failure of 38 months [9]. While these failures initially unnerved the team working on the project, reviews of literature reveal that such failures were by no means uncommon and had been faced and continue to be faced by each such group of surgeons and engineers working in the field of limb salvage. Biau et al reported mechanical failures including stem fractures and hinge pin failures in 7 out of 91 patients (7.7%) operated between 1972 and 1994 [10]. More recently in 2013, Nakamura et al [11] reporting on the Japanese early experience with the Kyocera limb salvage system revealed mechanical failures in 7 out of 82 distal femur resections (8.53%) including predominantly stem failures and one tibial tray breakage.
While the stem failures were beginning to present themselves and were being investigated, a number of refinements continued to be made in the period since 2004. The tibial baseplate acquired its rounded geometry (Fig. 7a) conforming to the tibial plateau. The important alignment mark on the stem was added (Fig. 7b) to enable correct rotational alignment of the implant. In mid-2005, bushes and a bumper manufactured from UHMWPE were introduced into the design (Fig. 7c) to minimize metal on metal articulation.
In early 2006, based on initial investigations into the failure location which was centered near the stem-bone junction, a decision was made to introduce a gradual change of diameter in the region and reduce stress concentration by introducing a fillet (Fig. 7d) with a liberal radius of curvature. This change was done based on standard good design principles and was perhaps the first engineering input to what had essentially been a surgeon-led project from inception.

With all the changes and refinements that had taken place over the years (Fig. 8a,b), the system in mid-2006 was fairly standardized based on a large patient experience of nearly 260 cases, standard condylar and intra-medullary dimensions, UHMWPE bushes and bumpers and a reliable hinge locking mechanism.
What however concerned the entire team was that the intramedullary stems continued to fail at the stem-bone junction and even the reduced stress concentration with the filleted design did not seem to work (Fig. 8c).
It was at this point that the engineering team at Sushrut-Adler brought in a new level of seriousness and application to understanding this problem better. Literature was extensively reviewed [12,13,14] to develop a better appreciation of the forces the implant was being subjected to. Resultant stresses on the implant cross sections were calculated and analyzed with reference to the materials being used. Based on the analytical work, it was clear that the stainless steel being used for these implants did not have the capability to withstand the continuous stresses being imposed on this implant in normal patient activities in the medium to long term. Better materials were needed. The team opted for titanium alloy as the material of choice for the ramedullary stems as a material with no biocompatibility issues given its long history of successful clinical use, the ability of the material to withstand the imposed stresses in this application with an adequate factor of safety and the lower modulus of elasticity which was perceived as a possible advantage.
The team opted for titanium alloy as the material of choice for the ramedullary stems as a material with no biocompatibility issues given its long history of successful clinical use, the ability of the material to withstand the imposed stresses in this application with an adequate factor of safety and the lower modulus of elasticity which was perceived as a possible advantage.
Titanium alloy is known to have its own difficulties in processing and is not an easy material from a manufacturing standpoint. Fortunately, the engineering and manufacturing teams at Sushrut-Adler had developed strong experience in working with this alloy due to their previous history with successful development and commercialization of spine implants manufactured from titanium alloy and these challenges were not difficult to overcome.
The change of materials and the expected solution to the difficult stem failure issue thus opened the way for the team of surgeons and the Sushrut-Adler engineers to take the next step of modularizing the system paving the way for more widespread use. The difficulties of custom-manufacturing implants by this time were well understood and the constraint imposed on an operating surgeon working with an implant of fixed size was not desirable. Modularity enabled a surgeon to intra-operatively select the most optimum surgical margin for the excision with no concerns about having an implant size that would adapt to the length of the resection.
The surgeons’ need for modularity resulted in many months of manufacturing trials at Sushrut-Adler as the necessary self-locking tapers for the modular components were designed and proven through the manufacturing process.
The final standardized condylar dimensions enabled the team to opt for superior Cobalt Chrome alloy investment castings for the condylar components thus gaining better articulation properties with the UHMWPE components.
The culmination of all these efforts resulted in the first patient implanted with the ResTOR modular resection prosthesis in a limb salvage procedure in late 2006. The modular system was commercialized in early 2007 for distal femur and proximal tibia resections. The addition of an upper limb system and a proximal femur resection system over the next few years enabled a complete portfolio of solutions.
It may be argued, with hindsight, that the inception of this project in 1999-2000 was with a compromised implant. However, as cogently argued by Dr. Agarwal ten years later [9], many patients benefited even with these compromised implants, the failure rate of around 15% was not viewed as catastrophic and was considered acceptable in a situation where an expensive implant was not an option and where amputation or rotationplasty would have been the only alternatives for the patient. The limb salvage procedure allowed many children to continue with education and adults to remain employed. Icing on the cake came in the form of the prestigious Golden Peacock Innovation Award in 2010 which recognized this as a major health-care initiative.
The ResTOR modular resection prosthesis system since 2007 has contributed to cost-effective limb salvage surgery of more than 2000 patients in India and a number of other countries [17] with prosthesis survivorship rates comparable to those reported in literature [15,16]. As a case in point, the Tata Memorial experience of 88% implant survivorship at five years with total femoral replacement [16], a specially challenging procedure with extensive resection does great credit to the team of surgeons and engineers who worked on this project. As implant survivorship improves and a greater number of patients experience disease-free survivorship with continuously improving surgeon experience, the ResTOR team continues to face newer challenges related to the increased demands on the implant.
While many improvements have been made and will continue to be made, as global experience with limb salvage implants has shown, the demands placed on these implants are immense and the way forward promises an abundance of challenges to be faced and problems to be solved.
Note
The author was privileged to be associated with this program right from inception till date and will remain forever grateful for the opportunities this program has provided to learn, develop and evolve. The team of engineers who have contributed at various stages are too numerous to name and their efforts will always be remembered and recognized by the surgeons who care for patients with these difficult conditions..
References
1. Mirabello L, Troisi RJ, Savage SA. International osteosarcoma incidence patterns in children and adolescents, middle ages and elderly persons. Int J Cancer. 2009 Jul 1;125(1):229-34..
2. Simon MA, Aschliman MA, Thomas N, Mankin HJ. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1986 Dec;68(9):1331-7.
3. Enneking WF, Spanier SS, Goodman MA. A System for the surgical staging of musculo-skeletal sarcoma. Clin. Orthop., 153;106-120, 1980.
4. Springfield DS, Schmidt R, Graham-Pole J, Marcus RB Jr, Spanier SS, Enneking WF. Surgical treatment for osteosarcoma. J Bone Joint Surg Am. 1988 Sep;70(8):1124-30.
5. Puri A. The “ODYSSEY”: “Orthopaedic Oncology” – My journey thus far! Journal of Bone and Soft Tissue Tumors May-Aug 2015; 1(1):3-5
6. Agarwal M, Anchan C, Shah M, Puri A, Pai S. Limb salvage surgery for osteosarcoma: effective low-cost treatment. Clin Orthop Relat Res. 2007 Jun;459:82-91.
7. Agarwal M, Puri A. Limb Salvage for malignant primary bone tumours: current status with a review of literature. Indian J Surg 2003;65:354-60.
8. Bos G, Sim F, Pritchard D, Shives T, Rock M, Askew L, Chao E. Prosthetic replacement of the proximal humerus. Clin Orthop Relat Res. 1987 Nov;(224):178-91.
9. Agarwal M, Gulia A, Ravi B, Ghyar R, Puri A. Revision of broken knee megaprostheses: new solution to old problems. Clin Orthop Relat Res. 2010 Nov;468(11):2904-13..
10. Biau D, Faure F, Katsahian S, Jeanrot C, Tomeno B, Anract P. Survival of total knee replacement with a megaprosthesis after bone tumor resection. J Bone Joint Surg Am. 2006 Jun;88(6):1285-93.
11. Nakamura T, Matsumine A, Uchida A, Kawai A, Nishida Y, Kunisada T, Araki N, Sugiura H, Tomita M, Yokouchi M, Ueda T, Sudo A. Clinical outcomes of Kyocera Modular Limb Salvage system after resection of bone sarcoma of the distal part of the femur: the Japanese Musculoskeletal Oncology Group study. Int Orthop. 2014 Apr;38(4):825-30.
12. Perry J, Antonelli D, Ford W. Analysis of knee-joint forces during flexed-knee stance. J Bone Joint Surg Am. 1975 Oct;57(7):961-7.
13. Paul JP. Approaches to Design – Force actions transmitted by joints in the human body. Proc. R. Soc. Lond. B. 1976; 192: 163-172.
14. Taylor SJ, Walker PS, Perry JS, Cannon SR, Woledge R. The forces in the distal femur and the knee during walking and other activities measured by telemetry. J Arthroplasty. 1998 Jun;13(4):428-37..
15. Puri A, Gulia A. The results of total humeral replacement following excision for primary bone tumour. J Bone Joint Surg Br. 2012 Sep;94(9):1277-81..
16. Puri A, Gulia A, Chan WH. Functional and oncologic outcomes after excision of the total femur in primary bone tumors: Results with a low cost total femur prosthesis. Indian J Orthop. 2012 Jul;46(4):470-4.
17. Data on file at Adler.
| How to Cite this article: Sarangapani R. From TMH-NICE to ResTOR: An Eventful Journey. Journal of Bone and Soft Tissue Tumors May-Aug 2015; 1(1):40-44. |
(Abstract) (Full Text HTML) (Download PDF)