A Rare Recurrent Chondromyxoid Fibroma of the Proximal Tibia in an Adolescent Female
Original Article | Volume 6 | Issue 3 | JBST September – December 2020 | Page 16-19 | Ashish Kumar Goyal, Abhishek Vaish, Raju Vaishya, Pankaj Baweja DOI: 10.13107/jbst.2020.v06i03.34
Author: Ashish Kumar Goyal[1], Abhishek Vaish[1], Raju Vaishya[1], Pankaj Baweja[2]
[1]Department of Orthopaedics and Joint Replacement Surgery, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi, India.
[2]Department of Pathology, Indraprastha Apollo Hospital, Sarita Vihar, New Delhi, India.
Address of Correspondence
Dr. Ashish Kumar Goyal, Department of Orthopaedics and Joint Replacement Surgery, Indraprastha Apollo Hospitals, Sarita Vihar, New Delhi – 110 076, India.
E-mail: drgoyal41@gmail.com
Introduction: Lytic lesions of the bone are often seen in children and young adults. These are usually benign but sometimes are locally aggressive bone tumors. Lesser known causes of lytic lesions are chondromyxoid fibroma (CMF) and its recurrence is very rare. The accepted treatment for CMF is surgical curettage with bone grafting and the review of the literature shows that recurrence rate is 3–22%.
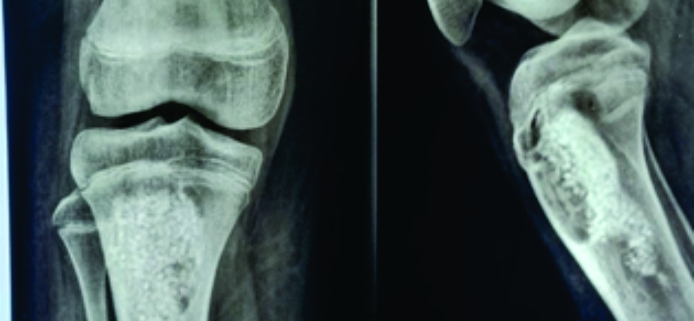
Case Report: We present a rare case of an adolescent girl of 14 years who presented with a recurrent bone tumor of the proximal tibia, after 4 years of the primary curettage. It turned out to be a CMF. She presented with swelling over the right upper leg for the past month. It was gradual in onset, progressive, and non-radiating in nature. There was no history of trauma. She had had a similar complaint 4 years back in 2016, for which she was operated elsewhere, where curettage and synthetic bone substitutes were used for filling the bone cavity. She was taken up for surgery for extended curettage and bone cementing. The histopathological examination was suggestive of CMF. Subsequent follow-up, she reported complete resolution of symptoms with a pain-free range of knee movements and no radiological signs of recurrence.
Conclusion: The accepted treatment for CMF is surgical curettage with bone grafting, but the recurrence rate is 3–22%.
Keywords: Chondromyxoid fibroma, benign lesions, tibia, recurrence.
Reference:
1. Berg E, Sokolay M. Diagnosis and management of lytic lesions in bone. JAMA 1982;247:2099.
2. Canale ST, Beaty JH, Campbell WC. Campbell’s Operative Orthopaedics. St. Louis, MO: Mosby; 2012. p. 860-4.
3. Vargas B. Orthopedic Surgery for Fibrous Dysplasia. Background, Pathophysiology, Etiology. New York: Medscape; 2019. Available from: https://www.emedicine.medscape.com/article/1255262-overview. [Last accessed on 2020 Aug 22].
4. Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Giant cell tumor of bone: Risk factors for recurrence. Clin Orthop Relat Res 2010;469:591-9.
5. Bhamra JS, Al-Khateeb H, Dhinsa BS, Gikas PD, Tirabosco R, Pollock RC, et al. Chondromyxoid fibroma management: A single institution experience of 22 cases. World J Surg Oncol 2014;12:283.
6. Vaishya R, Agarwal A, Gupta N, Vijay V. Fibrocartilaginous dysplasia of the bone: A rare variant of fibrous dysplasia. Cureus 2016;8:e448.
7. Hahn SB, Kim SH, Cho NH, Choi CJ, Kim BS, Kang HJ. Treatment of osteofibrous dysplasia and associated lesions. Yonsei Med J 2007;48:502-10.
8. Rui J, Guan W, Gu Y, Lao J. Treatment and functional result of desmoplastic fibroma with repeated recurrences in the forearm: A case report. Oncol Lett 2015;11:1506-8.
9. Hasan O, Ali M, Mustafa M, Ali A, Umer M. Treatment and recurrence of giant cell tumors of bone-a retrospective cohort from a developing country. Ann Med Surg (Lond) 2019;48:29-34.
10. Bush JB, Sweeney JP, Robison JE, DeMoss B, Meyer MS. Chondromyxoid fibroma of the radial shaft treated with nonvascularized fibular autograft. Am J Orthop (Belle Mead NJ) 2010;39:30-4.
11. Castle JT, Kernig ML. Chondromyxoid fibroma of the ethmoid sinus. Head Neck Pathol 2011;5:261-4.
12. Fomete B, Adeosun OO, Awelimobor DI, Olayemi L. Chondromyxoid fibroma of the mandible: Case report and review of the literature. Ann Maxillofac Surg 2014;4:78-80.
13. Wu CT, Inwards CY, O’Laughlin S, Rock MG, Beabout JW, Unni KK. Chondromyxoid fibroma of bone: A clinicopathologic review of 278 cases. Hum Pathol 1998;29:438-46.
14. Park HR, Lee IS, Lee CJ, Park YK. Chondromyxoid fibroma of the femur: A case report with intra-cortical location. J Korean Med Sci 1995;10:51-6.
15. Jamshidi K, Mazhar FN, Yahyazadeh H. Chondromyxoid fibroma of calcaneus. Foot Ankle Surg 2013;19:48-52.
16. Di Giorgio L, Touloupakis G, Mastantuono M, Vitullo F, Imparato L. Chondromyxoid fibroma of the lateral malleolus: A case report. J Orthop Surg (Hong Kong) 2011;19:247-9.
17. Ralph LL. Chondromyxoid fibroma of bone. J Bone Joint Surg Br 1962;44:7-24.
18. Vaishya R, Agarwal AK, Vijay V. ‘Salvage treatment’ of aggressive giant cell tumor of bones with denosumab. Cureus 2015;7:e291.
| How to Cite this article: Goyal AK, Vaish A, Vaishya R, Baweja P| A Rare Recurrent Chondromyxoid Fibroma of the Proximal Tibia in an Adolescent Female | Journal of Bone and Soft Tissue Tumors | September-December 2020; 6(3): 16-19. |